THE MALABSORPTION AND LACTOSE INTOLERANCE
Products for lactose intolerant
Pathophysiology, diagnosis and therapeutic approach
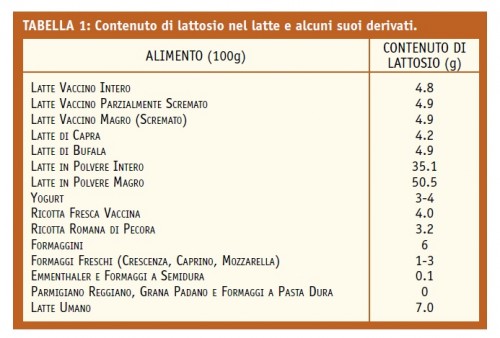
Lactose is a disaccharide composed of one molecule of glucose and one galactose combined with beta-glycosidic bond. It is synthesized by the mammary glands and is the main sugar in milk of most mammals. In human milk is about 40% of daily energy intake of the infant and it is estimated that one liter of cow's milk contains about 50 g of lactose. In contrast, the derivatives of the milk will contain variable amounts, inversely proportional to the degree of aging of the product: during this process, in fact, the lactose is fermented by lactic acid bacteria and therefore already semi-hard cheeses, such as Emmentaler, contain levels of lactose very low while hard cheeses, such as Parmigiano Reggiano, contain near-zero levels. Lactose is found also in many food preparations since it promotes good mixing of dyes and additives, is contained in candy, baked goods, breakfast cereals, sauces, puddings, meats, prepared for soup, potato dumplings, canned foods. Finally, it is used as an excipient in drugs and dietary supplements, but in concentrations of the order of a milligram, therefore negligible.
Lactose and Lactase
Lactose digestion occurs in the small intestine by the lactase, a protein expressed at the apex of the villi, fingerlike protrusions that increase the total surface area and therefore a capacity to absorb bowel weave. The cells lining the villi, in turn, are protrusions of the apical side with the seiche purposes defined brush border of the villi. The lactase has two active sites: the first hydrolyzes the lactose in the two monosaccharides glucose and galactose, making them absorbable by the intestinal mucosa, the second hydrolyzes florizina glycosphingolipids and some food, which makes the expression of the enzyme required throughout the course of life.
The hypolactasia
When the intestinal lactase activity is not sufficient to digest lactose introduced with the feed, it is called hypolactasia or lactase deficiency, a condition that causes malabsorption of lactose. The activity of lactase in the small intestine is measurable already the 8th week of gestation and increases until the 34th week, the levels of lactase in the intestine are highest at birth, but after weaning, the expression of the enzyme undergoes a gradual and progressive reduction in most mammals (fi is lost no to 75-90% of the enzyme) determining hypolactasia primary. The resulting malabsorption of lactose generally occurs no earlier than 6-7 years of age but sometimes it is also much later, showing a steady increase in prevalence even in the age groups above 65 years. The kinetics of the reduction and the magnitude of the residual lactase show considerable variability between different ethnic groups and even between individuals. Please note that the reduction fi no to 50% of the lactase is still suffi cient to ensure effective digestion of lactose. There are also other forms of hypolactasia. The hypolactasia congenita is a rare autosomal recessive disorder, characterized by severe diarrhea with watery stools event since the first intake of milk by the newborn; persists throughout life and requires the complete exclusion of lactose sources of supply. The secondary hypolactasia occurs, however, when a damage of the mucosa of the small intestine causes a temporary lactase deficiency; typically, all diseases of the small intestine, such as celiac disease or Crohn's disease in localization enteral, are in capable of causing a secondary deficiency of lactase, but most commonly bacterial or viral infections, parasitic infestations, such as a giardiasis, or pharmacological treatments induce a transient loss of enzyme in the areas of mucosa affected by the inflammatory process or infectious. It is obviously a reversible condition, which requires the exclusion of the sources of lactose from the diet only until it is restored the normal structure of the intestinal mucosa. We'll focus sull'ipolattasia primary, taking stock of the current knowledge about the mechanisms that lead to the appearance of symptoms, tests to make the diagnosis and management of disease in clinical practice.
Primary hypolactasia: diffusion and genetic basis
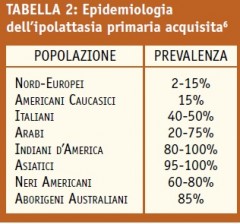
The primary hypolactasia is an extremely prevalent condition in the world population, but with substantial variations between different ethnic groups, the prevalence of the disease is minimal in populations in northern Europe and in the groups that they descend from, and is particularly high in Asia, Africa and Australia. From the phylogenetic point of view, the "normality" is the loss of the expression of lactase, defined as "non-persistent". In fact, in human life, like other mammals, the power supply is based exclusively on breast milk for the first few months of life. It is therefore guessed how the regulation of the expression of the lactase gene may predict its progressive decline in later stages of life. However, the genotype that determines the persistence of lactase, is found only in populations in northern Europe, their descendants, in some African and Arab nomadic tribes. In Europe, the persistence or non-persistence of the expression of lactase is associated with the so-called polymorphism punctiform C/T13910, namely the substitution of a single nucleotide base in a DNA sequence which plays regulatory activity on the lactase gene: the CC genotype is associated to hypolactasia (lactase residual is about 10% compared to the levels of the birth), while the TT genotype in persistence of lactase activity. The presence of a genotype CT, instead, predisposes to the presence of intermediate levels of expression.
Hypolactasia, malabsorption and intolerance
In the presence of hypolactasia occurs malabsorption of lactose. The proportion of lactose is not digested and not absorbed by the small intestine reach the colon, an organ not able to absorb the sugars. Here is fermented by the resident bacterial flora with production of short chain fatty acids (butyrate, acetate, propionate), water and gas (CO2, H2, CH4, N2). The resulting appearance of symptoms, the so-called syndrome lactose intolerance, is directly dependent on this process: short-chain fatty acids, physiological source of energy for the cells of the colon, if present in high concentrations cause pain both for acidification of the content the bowels both for direct mucosal irritative effect, which causes also an 'acceleration of the motor activity of the colon and then diarrhea, for a consequent lower efficiency of the mechanisms of water absorption; excessive fecal content in water is also caused its release during the process of fermentation of sugar, and finally, the excessive production of gas causes the symptoms of so-called "gas-relative", such as bloating, flatulence and abdominal distension which, if excessive, can favor the onset of pain . In this regard, it should be noted that the aforementioned cascade of events is identical to any form of sugar that is not absorbed by the small intestine: fructose, mannitol, food sweeteners, lactulose, including the fi bre food. This accounts for the fact that the perception by the patient about symptoms of the causal role of various foods. introduced with food is often incorrect and the abolition of certain foods from the diet, consequently, it is often useless, if not even harmful. Not all subjects with lactose malabsorption, however, have the syndrome of intolerance. The reasons why this happens are partially clear. Surely, the amount of residual lactase expressed by cells of the small intestine is the main parameter, but of fundamental importance are also: - the amount of lactose introduced with the feed, as in subject malassorbente is known that the greater the load oral, greater is the risk of developing symptoms, the composition of the meal, as they are able to influence the gastric emptying time. The nutrients most effective in slowing gastric emptying are lipids, followed by protein, fiber, and carbohydrates; the intestinal transit time, as it can affect the contact time between lactose and lactase. Acceleration of transit reduces the possibility of contact between enzyme and substrate preventing the residual lactase to hydrolyze the lactose. More recently, it has also been studied the importance of other factors that may contribute to the onset of the syndrome by intolerance in subjects with lactose malabsorption. For example, a key parameter is represented by the visceral sensitivity. Subjects "hypersensitive", that is characterized by low sensitivity thresholds, can be perceived as annoying a stimulus applied at the level of the colon that in subjects normosensibili is asymptomatic and thus can react with discomfort to the effects in the intestine of intraluminal factors. In addition, the qualitative and quantitative characteristics of the bacterial flora of the colon may play an important role. In fact, it is likely that the extent of fermentation processes that take place in the colon depends largely on the composition of the flora farmhouse. Finally, psychological factors can greatly affect the perception of symptoms and should be taken into serious consideration in the evaluation of disorders reported by the patient.
The consequences of intolerance and health risks
Lactose intolerance, alleged or real, implies on the part of patients spontaneous exclusion from the diet of milk and its derivatives. This attitude represents a protective mechanism put in place by patients to prevent gastrointestinal disorders defendants, not always with good reason, the assumption of such products. This leads to an increased risk of developing nutritional deficiencies. In fact, the removal of it from milk and dairy products makes it very difficult to meet the daily requirements of calcium. This bone level hinders the achievement of an adequate level of mineralization at a young age and encourages the development of osteoporosis in perimenopausal age, postmenopausal and senile. In addition, it was recently shown that the perception by the patient to be the bearer of lactose intolerance is associated with hypertension and diabetes mellitus type 218 and as the habitual consumption of milk and dairy products is associated with a lower incidence of colon cancer.
Conclusions
In conclusion, the lactose malabsorption is a condition widespread in Italy, but much less frequent syndrome intolerance. In fact, people that eliminate milk and cheese from their diet, mistakenly believe that they are the cause of their ailments, are undoubtedly more numerous than those actually carriers of the syndrome. The role of the physician is, therefore, essential to prevent potential nutritional deficiencies as it must clarify the actual relationship between disorders and lactose. The lactose breath test, a simple non-invasive test, is used to confirm or exclude the presence of malabsorption and, with proper precautions, it can diagnose the syndrome of intolerance. An accurate diagnosis is critical to set adequate dietary measures that on the one hand avoid nutritional deficiencies and, secondly, are effective in improving the symptoms.
Scientific investigation by Michele Di Stefano, Medical Clinic 1, Fondazione IRCCS Policlinico "San Matteo", Pavia
Lactose intolerance
Products for lactose intolerant
